Less administration
Administrative workload in primary care is continuously increasing. A significant amount of time is spent collecting medical information, processing documents, and coordinating care among different providers.
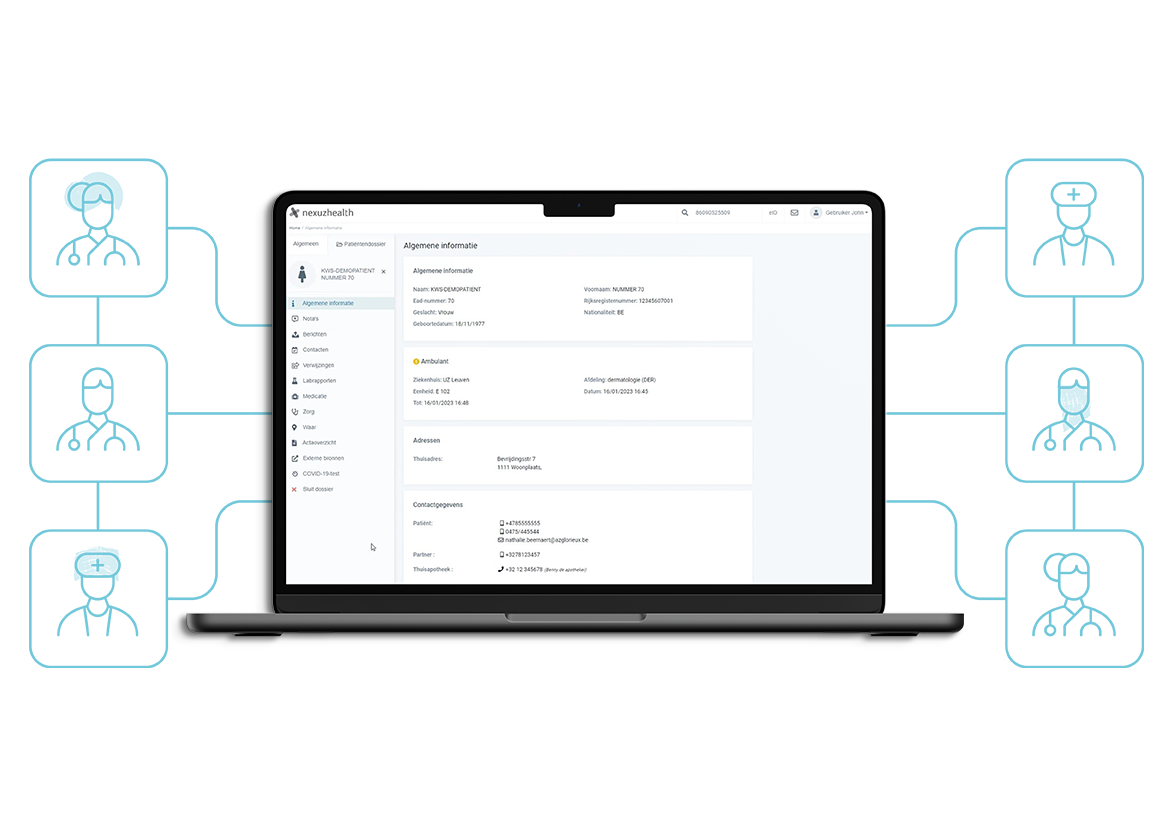
With a digitally accessible patient record, GPs can quickly find the necessary information, reducing the time spent on searching for data. This means more time for patient care and less administrative hassle.
A concrete example: a patient visits a GP a few days after gallbladder surgery, complaining of abdominal pain. Thanks to hospital record access, the GP can immediately review the surgical report, lab results, and discharge letter. Any complications during surgery are also visible, allowing the GP to determine immediately whether additional examinations are needed.


-2.png?width=1534&height=1200&name=Afbeeldingen_Consult%20(1)-2.png)